Soap Notes Electronic Medical Records
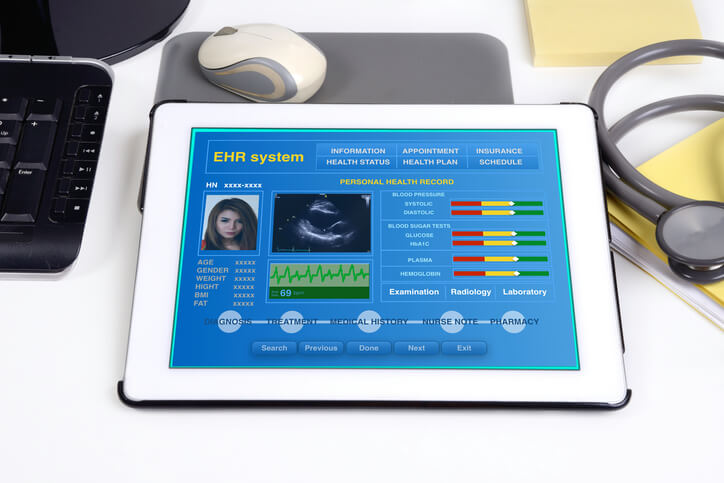
With the soap notes structure, they can quickly log onto their computer or medical tablet, access the patient’s records, and scroll down to the “plan” section where that information would be highlighted. clear, concise, and much less likely to result in miscommunication between healthcare providers. Qnotes office emr™ is our locally-installed electronic medical records software. notes from pdq are instantly typed error-free, and filed away safe and secure in the emr. learn what quick notes will do for you, and see the top 10 reasons to buy quick notes today!. It’s a patient’s right to view his or her medical records, receive copies of them and obtain a summary of the care he or she received. the process for doing so is straightforward. when you use the following guidelines, you can learn how to.
An important part of patient electronic health records, soap notes should be legible and make use of professional jargon to serve as a common frame of reference. they should be written in the present tense. concise and specific. Your private medical record is not as private as you may think. here are the people and organizations that can access it and how they use your data. in the united states, most people believe that health insurance portability and accountabil. Will electronic medical records be safe? with the effort to digitize health records in the works, see if your electronic medical record will be soap notes electronic medical records safe. advertisement by: molly edmonds in today's world, many people think nothing of oversharing. Search for results at sprask. find info on sprask. com.

Fast Results
Soap notes are an essential piece of information about the health status of the patient as well as a communication document between health professionals. the structure of documentation is a checklist that serves as a cognitive aid and a potential index to retrieve information for learning from the record. An emr or ehr contains a wide variety of information like treatment history, medical records, patient progress, etc. soap finds its usage in recording patient progress. soap or soap notes as they are widely called also find extensive usage in veterinary practices. it is a way for clinics to record, document, and store patient’s medical. Find electronic soap notes on topsearch. co. topsearch. co updates its results daily to help you find what you are looking for. In the united states, you have the legal right to obtain any past medical records from any hospital or physician. retrieving old records, even those stored on microfilm, can be a simple process, depending on the hospital's policy for storin.
Soap notes are most often found in a patient’s electronic health record. seeing as other medical professionals will have access to the records of the patient they’re treating, reading soap notes that are structured in an easy-to-read, organized way will mean they’ll know exactly what they need to do to help the patient. Patient records are anything on any media which has been gathered as a result of the work of the employee ( the physiotherapist) pomr is based upon a collection of data formulation of problems to develop a suitable treatment programme. it is unlawful to act 'in the best interests' of the patient without consent. treatment given to incapacitated adults without consent is only in cases of a. Soap notes. today, the soap note an acronym for subjective, objective, assessment, and plan is the most common method of documentation used by providers to input notes into patients’ medical records. they allow providers to record and share information in a universal, systematic and easy-to-read format. many elements of modern health.
Electronic medical records. save time & get quick results. visit today & quickly get more results on fastquicksearch. com!. Consumer's rights with respect to their medical records hhs hipaa home for individuals your medical records this guidance remains in effect only to the extent that it is consistent with the court’s order in ciox health, llc v. azar, no. How to write medical soap notes. in the medical worls, "soap" stands for subjective, objective, assessment and plan. the soap note is a daily notation of a patient's condition, progress and immediate plan for diagnosis and treatment. a well. There are a few benefits of electronic medical records. see reasons why paper records will be phased out due to the benefits of electronic medical records. advertisement by: molly edmonds medical professionals in the united states have inve.
Soap Notes On The App Store
Soap notes are used for admission notes, medical histories and other documents in a patient’s chart. many hospitals use electronic medical records, which often have templates that plug information into a soap note format. most healthcare clinicians including nurses, physical and occupational therapists and doctors use soap notes. If dietitians use soap (subjective, objective, assessment, and plan) or adime (assessment, diagnosis, intervention, monitoring, and evaluation) notes, they’re available with the emr as well. patalano leaves room at the bottom of the patient feedback form where she can type a personal note, such as “great job soap notes electronic medical records on snacking this month” or. Practicefusion is a cloud-based electronic health records platform for medical practices of all sizes in the u. s. practicefusion currently services over 20,000 medical practices in the u. s. practicefusion’s platform includes templates for medical charts and soap notes. Soap notes is a robust patient manager app that is specifically designed to allow for quick, accurate soap notes for each patient's visit. soap notes is ideal for any person who must manage detailed notes for each patient visit and needs an app that will enter the notes quickly, and accurately.
Whether you're interested in reviewing information doctors have collected about you or you need to verify a specific component of a past treatment, it can be important to gain access to your medical records online. this guide shows you how. Incomplete progress notes (for example, unsigned, undated, insufficient detail) unauthenticated medical records (for example, no provider signature, no supervising signature, illegible signatures without a signature log or attestation to identify the signer, an electronic signature. As a therapist, there’s a variety of reasons soap notes electronic medical records why you want to take thorough subjective, objective, assessment and planning (soap) notes. you’ll be taking notes for a client’s electronic health record (ehr), which other healthcare providers w.
Post a Comment for "Soap Notes Electronic Medical Records"